Direct Patient Care Rotations
Goals, Objectives and Assessment Tools and Resources
1. Direct Patient Care Rotation Goals and Objectives [click to view as a PDF]
The following goals and objectives pertain to all direct patient care rotations and can be found in the rotation summary for each direct patient care rotation. Rotation-specific goals and objectives outlined in the rotation summaries are considered in addition to the overall direct patient care rotation goals and objectives. The resident will be assessed on their ability to meet these goals and objectives during each direct patient care rotation and throughout the residency year. Given the specialized nature of the clinical orientation rotation and the precepting skills rotation, these rotations have their own goals and objectives which can be found in their respective rotation summaries.
Direct Patient Care Rotation Goals and Objectives
Goals
- To develop and integrate the knowledge required to provide evidence-based patient care as a member of the interprofessional team.
- To demonstrate the necessary skills required to perform patient-centred clinical assessments and establish evidence-based care plans incorporating the principles of shared decision-making in collaboration with other health care professionals.
- To demonstrate the attitudes and behaviours characteristic of a mature health care professional.
- To demonstrate the necessary skills to manage their own practice of pharmacy, effectively carry out professional duties and advance their learning.
Objectives
The resident will be able to:
- Relate knowledge of pathophysiology, risk factors, etiology and clinical presentation of common medical conditions including symptoms, physical assessment, relevant diagnostics and laboratory findings to patient-specific findings to make appropriate clinical assessments and care plans. [CPRB 3.1.1.b]
- Relate knowledge of pharmacology, pharmacokinetics and therapeutics to patient-specific findings and integrate best available evidence to make appropriate clinical assessments and care plans. [CPRB 3.1.1.b, 3.1.2.a.b.c]
- Apply safe medication practices to clarify, manage and improve medication use for individual patients and groups of patients. [CPRB 3.2.5, 3.2.6, 3.3.2]
- Place a high priority on and be accountable for selecting and providing appropriate care to patients who are most likely to experience drug therapy problems. [CPRB 3.1.1.a, 3.1.7]
- Establish a respectful, professional and ethical relationship with the patient and/or their caregivers, by engaging in empathetic, compassionate, non-judgemental, culturally safe and tactful conversations. [CPRB 3.1.4, 3.1.8.a]
- Accurately gather, evaluate and interpret relevant patient information from all appropriate sources in an organized, thorough and timely manner, including effectively eliciting patient history and performing assessments. [CPRB 3.1.8.d.e]
- Develop a prioritized medical problem list and describe the active issues that are responsible for the patient’s admission or clinic visit. [CPRB 3.1.8.f]
- Identify, prioritize and justify a list of patient-specific drug therapy problems. [CPRB 3.1.8.c, 3.2.4]
- Establish and incorporate the patient’s desired outcome(s) of therapy and advocate for the patient in meeting their health-related needs. [CPRB 3.1.5, 3.1.6, 3.1.8.b.f]
- Identify, assess and justify a list of reasonable therapeutic alternatives and integrate best available evidence into clinical decision-making with consideration of drug efficacy, safety, patient factors, administration issues and cost. [CPRB 3.1.2.b.c, 3.1.8.d.e.f]
- Establish a patient care plan and implement recommendation(s) that include consideration of the patient’s goals and the roles of other team members; and incorporates the principles of shared decision making. [CPRB 3.1.1.d, 3.1.3.c, 3.1.6, 3.1.8.f.g]
- Proactively monitor drug therapy outcomes and revise patient care plans on the basis of new information. [CPRB 3.1.8.h.i]
- Establish and maintain effective inter- and intra-professional working relationships for collaborative care and provide safe and effective transfer of responsibility during care transitions. [CPRB 3.1.3.a.b.e.f]
- Proactively share and document information about care plans and any additional measures to optimize clinical decision-making, patient education and patient safety both verbally and in writing to team member(s), patient and/or caregiver(s), as appropriate. [CPRB 3.1.1.d, 3.1.8.i]
- Effectively respond to medication- and practice-related questions and educate others in a timely manner, select and navigate resources, utilize systematic literature search and critical appraisal skills to formulate a response shared verbally or in writing, as appropriate. [CPRB 3.1.2.a.b.c, 3.5.1.a.b.c.d.e]
- Demonstrate responsibility for own learning through refinement and advancement of critical thinking, scientific reasoning, problem solving, decision making and interprofessional skills to manage one’s own clinical practice and effectively carry out professional duties. [CPRB 2.1.5.3, 2.1.5.4, 3.1.1.c, 3.4.1]
- Demonstrate commitment to the profession, collaboration and cooperation with other health care workers and an understanding of the role of the pharmacist in the interprofessional team in the improvement of medication use for patients. [CPRB 2.1.5.6, 3.1.3.a.b.c.d, 3.2.2, 3.3.4]
Preceptor Orientation to New Direct Patient Care Rotation ITAR [Click to view Presentation Handout]
2. Direct Patient Care Rotation ITAR (In-Training Assessment of Resident) [Click to view Form]
During and at the end of the each direct patient care rotation (DPC), the resident will be assessed on their abilities in three core domains:
- Knowledge
- Skills (Provision of Pharmaceutical Care)
- Attitudes and Behaviours (Professional Characteristics)
These domains and their assessment criteria reflect the knowledge, skills, attitudes and behaviours required of residents to successfully complete the residency program and are hallmarks of professional clinical pharmacists. Each of these domains and their assessment criteria are linked to a Canadian Pharmacy Residency Board (CPRB) competency and associated requirement, which residents are expected to achieve by the end of the residency year.
Direct Patient Care ITAR Performance Rubrics
Below are the performance rubrics used in the DPC ITAR. These rubrics outline the levels of performance to which the resident will be assessed in the knowledge and skills domains. These rubrics can be used by both the resident and preceptor to understand the performance requirements for each level of performance in the DPC ITAR. They also allow for standardization of resident assessment across rotations and preceptors.
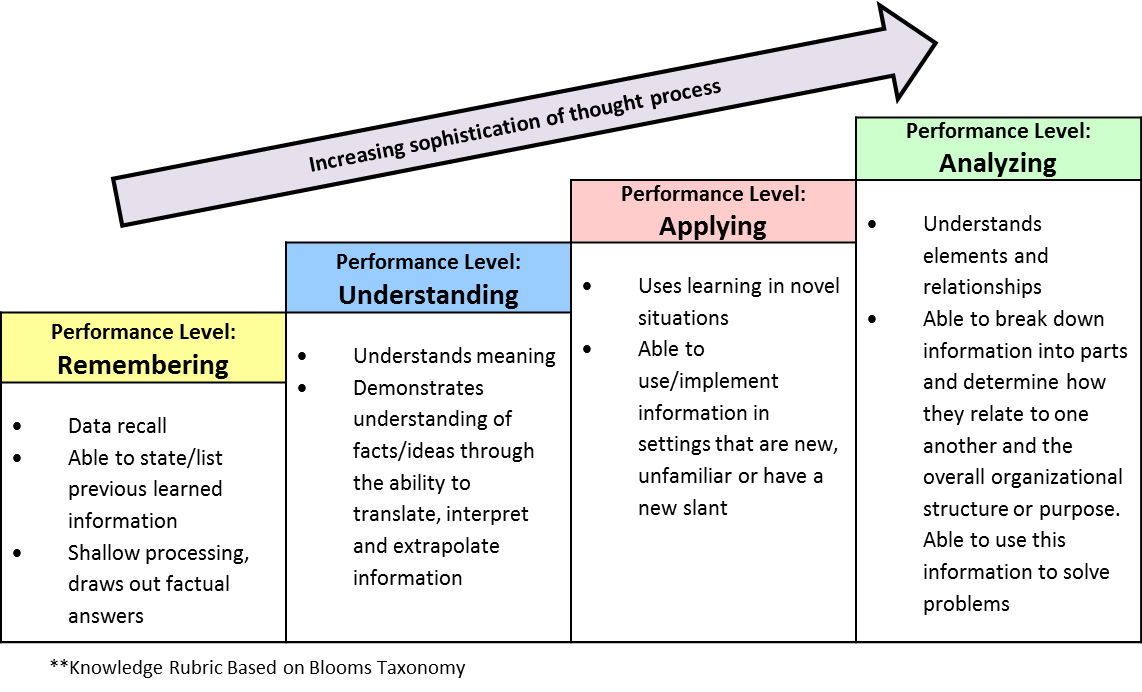
Knowledge Rubric [Click to view as PDF]
The Knowledge Rubric is based on Blooms Taxonomy. It outlines the levels of performance for each assessment criterion in the knowledge domain to which the resident will be assessed throughout the rotation. There are four levels of performance. These levels of performance reflect the stages of learning that an adult (i.e. resident) undertakes when acquiring, interpreting and relating new knowledge. They are ordered from basic (Remembering) to complex (Analyzing) and reflect a cumulative hierarchy whereby the resident has to master the more basic level of performance before moving to the more complex level of performance.
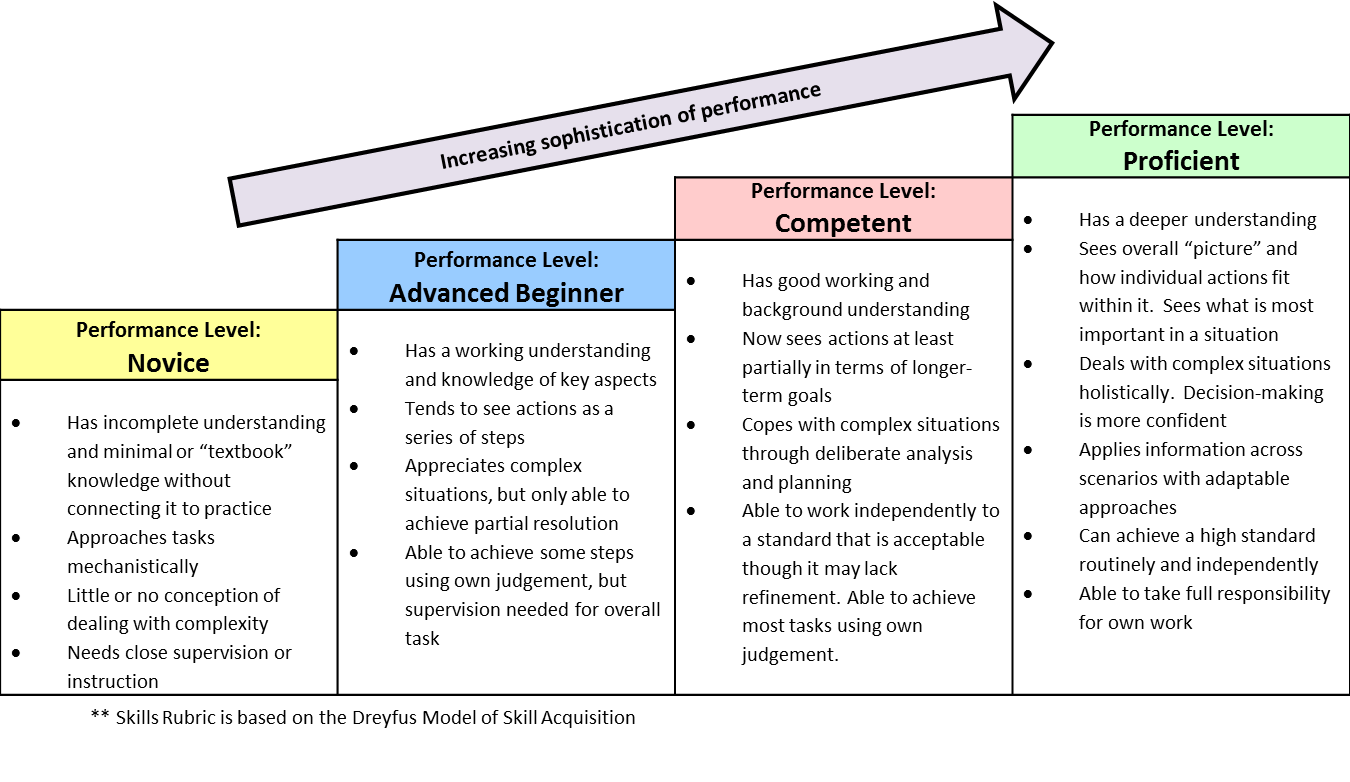
Skills (Provision of Pharmaceutical Care) Rubric [Click to view as PDF]
The Skills Rubric is based on the Dreyfus Model of Skill Acquisition. It outlines the levels of performance for each assessment criterion in the skills domain to which the resident will be assessed throughout the rotation. There are four levels of performance. These levels of performance reflect the stages of learning that an adult (i.e. resident) undertakes when learning a new skill. They are ordered from basic (Novice) to sophisticated (Proficient) and reflect a cumulative hierarchy whereby the resident has to master the more basic level of performance before moving to the more sophisticated level of performance.
Level of Patient or Problem Complexity Frame of Reference
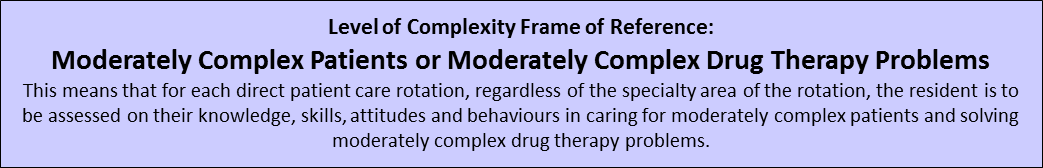
This means that for each direct patient care rotation, regardless specialty area of the rotation, the resident is to be assessed, using the DPC ITAR, on their knowledge, skills, attitudes and behaviours in caring for moderately complex patients and solving moderately complex drug therapy problems. Each performance level outlined in the Knowledge Rubric and Skills Rubric pertains to the resident’s ability to care for moderately complex patients and solve moderately complex drug therapy problems.
Assessing the Resident Using the DPC ITAR
When assessing the resident using the DPC ITAR:
- Each assessment criterion is associated with a description of the relevant components that pertain to that assessment criterion.
- Below each level of performance there is an example description of a resident’s performance as it relates to the particular performance level.
- When assessing the resident, the preceptor can use the example description and corresponding level of performance in the appropriate rubric to determine the resident’s level of performance at the mid-point and end of the rotation. Note that these levels of performance represent a cumulative hierarchy. This means, for example, that by assessing the resident as “competent” for a specific assessment criterion, the resident has already met the criteria for “novice” and “advanced beginner”.
- In the comment box below the assessment criterion, the preceptor should provide evidence and feedback to support the attained performance level.
- At the end of the assessment form, there is an opportunity to assess the resident on any rotation specific or resident personal rotation objectives that the preceptor or resident feels are not encompassed by the above assessment criteria.
Resident Expected Level of Performance [Click to view as PDF]
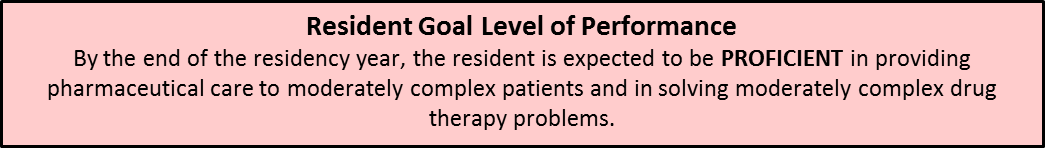
The table below outlines the goal level of performance for the resident throughout the residency year, based on the number of direct patient care rotations that they have completed or is in the process of completing. In some cases, residents should have achieved a particular level of performance by an early stage in the residency year, meaning that the remainder of the year is focused on refining and further developing the attained level of performance.
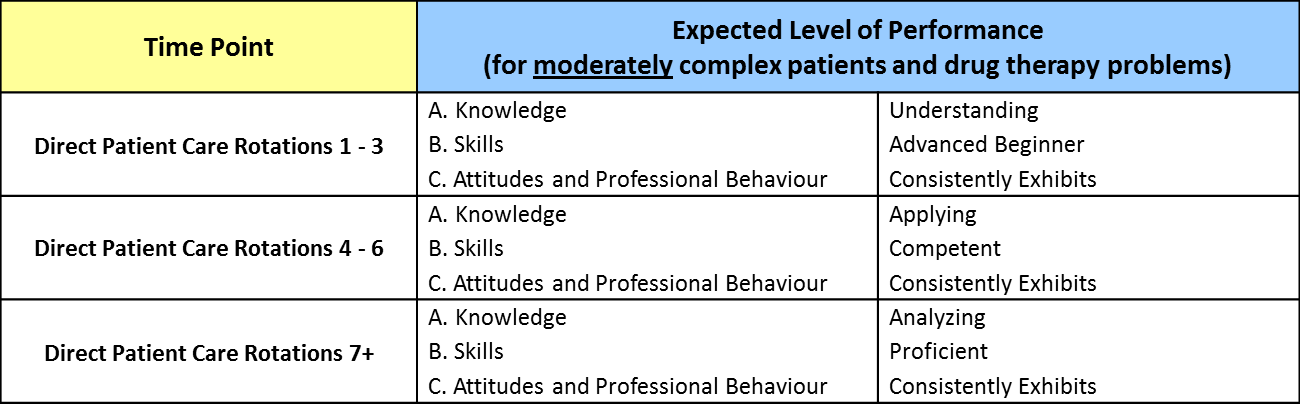
Note: There are 8 direct patient care rotations in this program. This includes all core (4 rotations) and elective (3 rotations) 4-week direct patient care rotations and the precepting skills rotation, which is a direct patient care rotation. The clinical orientation rotation is an orientation direct patient care rotation and is not included in the total number of direct patient care rotations in the table above. The expected level of performance for the clinical orientation rotation is outlined below. Direct Patient Care Rotation 1 in the table above is the resident's first 4-week direct patient care rotation.
How is this Table Used?
This table is to be used by the resident and preceptor as a guide to understanding the expected level of resident performance at various stages of the residency year.
- Residents can use this to better understand their current level of performance as it relates to the time point during the residency year and their progress towards meeting the goal level of performance. It can also help residents identify focus areas for improvement and further development.
- Preceptors can use this to better understand the resident’s current level of performance as it relates to how the resident is expected to be performing at that stage in the residency year. If a resident is not at the expected level of performance, then the preceptor can work with the resident to provide learning opportunities to further develop the required competency.
- The Program Coordinator will refer to this table to assess the resident’s progress towards meeting the goal level of performance throughout the residency year. When it is noted that the resident is not yet at the expected level of performance at a particular time point, the Program Coordinator will work with the resident and preceptor, as appropriate, to help the resident develop a learning plan to address the areas requiring further development and focus.
3. Clinical Orientation Rotation ITAR [Click to view Form]
This ITAR will be used to assess the resident at the end of the Clinical Orientation Rotation. The assessment criteria are taken directly from the clinical orientation rotation summary.
The Expected Level of Performance for the Clinical Orientation rotation is:
- Knowledge: Understanding
- Skills: Advanced Beginner
- Attitudes and Behaviours: Consistently Exhibits
4. Precepting Skills Rotation ITAR [Click to view Form]
This ITAR will be used to assess the resident at the end of the Precepting Skills Rotation. The assessment criteria are taken directly from the precepting skills rotation summary.
The Expected Level of Performance for the Precepting Skills rotation is based on the number of direct patient care rotations that the resident has completed as outlined in the Expected Levels of Performance table above.
-Last updated June 10, 2024